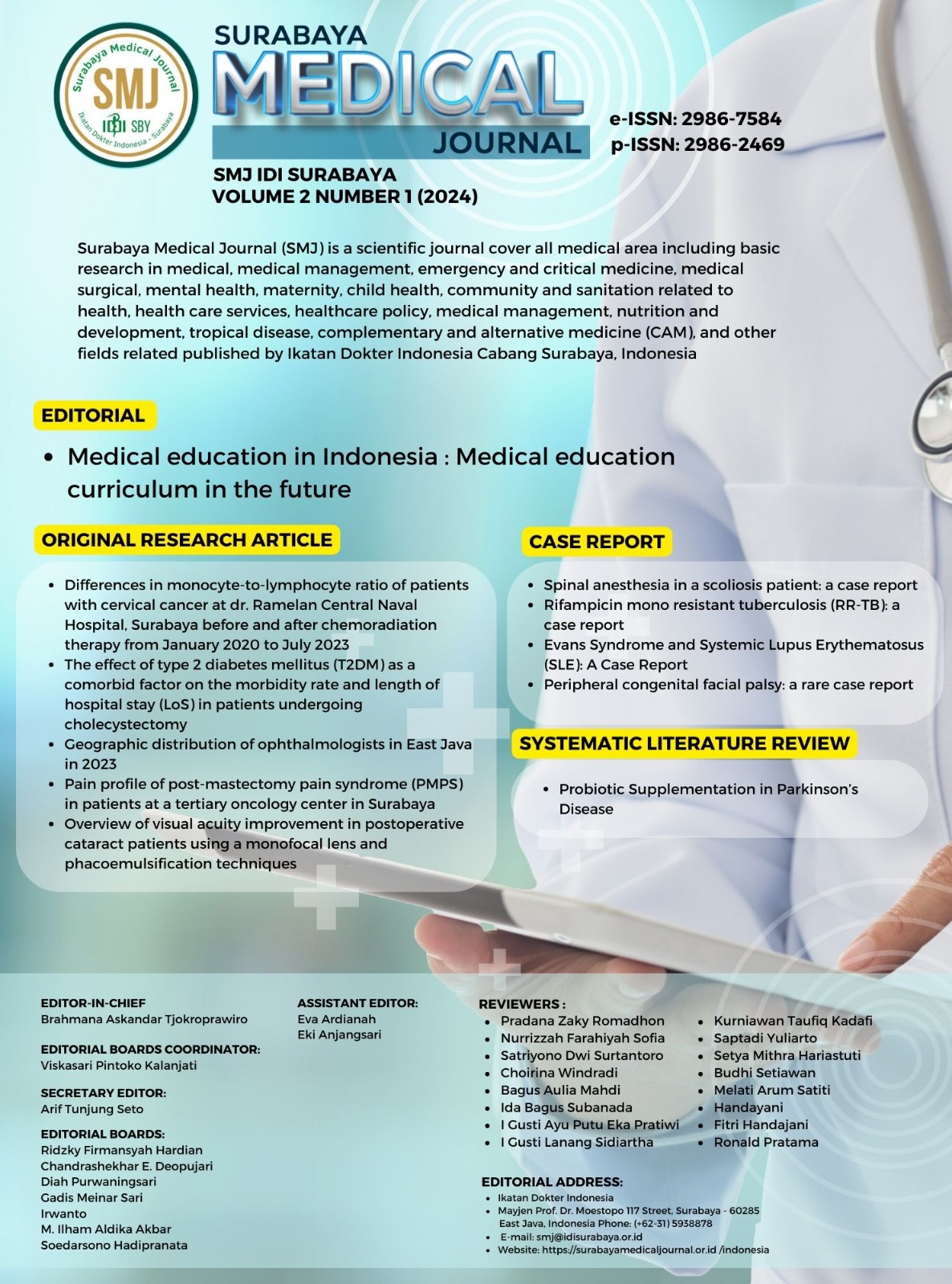
Rifampicin mono resistant tuberculosis (RR-TB): a case report
Rifampicin mono resistant tuberculosis
DOI:
https://doi.org/10.59747/smjidisurabaya.v2i1.38Keywords:
Tuberculosis, Pulmonary Tuberculosis, Drug-resistant TuberculosisAbstract
Introduction: Tuberculosis (TB) is a human disease caused by Mycobacterium tuberculosis. The bacteria is a rod-shaped and acid-resistant, hence it is also known as acid fast Bacilli. The disease mainly affects the lungs, making pulmonary disease the most common presentation of Tuberculosis. Despite advances in tuberculosis control and a decline in new cases and deaths, the disease remains a huge burden of morbidity and mortality worldwide. Diagnosis is at the forefront of TB management. Accurate diagnosis will be followed by appropriate management, thereby reducing mortality and morbidity from TB. Case Report: A 41-year-old male patient came to Puskesmas Kedurus after hospitalization at RSUD Dr. Soetomo after being diagnosed with TB-RO. Previously, the patient had a cough and weight loss for about 1 year, cough with greenish-yellow sputum, not containing blood. The patient began complaining about shortness of breath since 1 month ago, with the results of thorax photos and Real-Time Polymerase Chain Reaction (RT-PCR) supporting the diagnosis of Drug-resistant Tuberculosis. The patient received anti-tuberculosis drugs according to standard therapy for Multi-Drug Tuberculosis (MDR-TB) patients with a minimum treatment duration of 20 months. Conclusion: The risk factor for Tuberculosis in this patient was the surrounding community where the patient works daily with many coworkers who suffer from prolonged cough. The patient's prognosis is good if complaints are resolved immediately and anti-tuberculosis drugs was taken regularly. The patient still needs further education, especially regarding the cough etiquette and implementing healthy lifestyle in the household setting.
References
Adigun, R., Singh, R., 2024. Tuberculosis. StatPearls [Internet].
Altiner, A., Wilm, S., Däubener, W., Bormann, C., Pentzek, M., Abholz, H.H., Scherer, M., 2009. Sputum colour for diagnosis of a bacterial infection in patients with acute cough. Scand. J. Prim. Health Care 27, 70–73.
Astuti, V.W., Nursasi, A.Y., Sukihananto, 2019. Pulmonary tuberculosis prevention behavior improvement and structured-health education in Bogor regency. Enferm. Glob. 18, 285–302.
Bacelo, A.C., do Brasil, P.E.A.A., Cople-Rodrigues, C. dos S., Ingebourg, G., Paiva, E., Ramalho, A., Rolla, V.C., 2017. Dietary counseling adherence during tuberculosis treatment: A longitudinal study. Clin. Nutr. ESPEN 17, 44–53.
Behera, D., 2019. Complications of Pulmonary Tuberculosis. In: Tuberculosis. pp. 519–519.
Bernabe-Ortiz, A., Carcamo, C.P., Sanchez, J.F., Rios, J., 2011. Weight variation over time and its association with tuberculosis treatment outcome: A longitudinal analysis. PLoS One 6, 2–6.
Bommart, S., Charriot, J., Nagot, N., Vernhet-Kovacsik, H., Revel, M.P., Boissin, C., Bourdin, A., Tuaillon, E., 2021. Differentiating between active and latent tuberculosis with chest computed tomography. Diagn. Interv. Imaging 102, 605–610.
Caminero, J.A., Cayla, J.A., García-García, J.M., García-Pérez, F.J., Palacios, J.J., Ruiz-Manzano, J., 2017. Diagnosis and Treatment of Drug-Resistant Tuberculosis. Arch. Bronconeumol. 53, 501–509.
Campbell, I.A., Bah-Sow, O., 2006. Pulmonary tuberculosis diagnosis and treatment. Br. Med. J. 332, 1194–7.
Chakaya, J., Kirenga, B., Getahun, H., 2016. Long term complications after completion of pulmonary tuberculosis treatment: A quest for a public health approach. J. Clin. Tuberc. Other Mycobact. Dis. 3, 10–12.
Chopra, N., Halkur Shankar, S., Biswas, S., Ray, A., 2021. Pulmonary tuberculosis presenting as acute respiratory distress syndrome. BMJ Case Rep. 14, 1–4.
Chowdhury, K., Ahmad, R., Sinha, S., Dutta, S., Haque, M., 2023. Multidrug-Resistant TB (MDR-TB) and Extensively Drug-Resistant TB (XDR-TB) Among Children: Where We Stand Now. Cureus 15, 1–15.
Chowdhury, S., Chakraborty, P. pratim, 2017. Universal health coverage ‑ There is more to it than meets the eye. J. Fam. Med. Prim. Care 6, 169–170.
Chung-Delgado, K., Revilla-Montag, A., Guillén-Bravo, S., Bernabe-Ortiz, A., 2014. Weight variation over time and its relevance among multidrug-resistant tuberculosis patients. Int. J. Infect. Dis. 23, 20–24.
Dzhangaziev, B., Kulzhabaeva, A., Truzyan, N., Zhoroev, A., Otorbaeva, D., Temirbekov, S., Shahumyan, E., Davtyan, K., Isakov, T., 2020. New approach for tuberculosis contact tracing implemented in the two regions of Kyrgyz Republic during 2017-2018. J. Infect. Dev. Ctries. 14, 109S-115S.
Field, S.K., Escalante, P., Fisher, D.A., Ireland, B., Irwin, R.S., 2018. Cough Due to TB and Other Chronic Infections: CHEST Guideline and Expert Panel Report. Chest 153, 467–497.
Fu, H., Lewnard, J.A., Frost, I., Laxminarayan, R., Arinaminpathy, N., 2021. Modelling the global burden of drug-resistant tuberculosis avertable by a post-exposure vaccine. Nat. Commun. 12, 1–9.
Gibson, J., Donnan, E., Eather, G., 2018. Management of rifampicin mono-resistant tuberculosis in Queensland, Australia: a retrospective case series. Respirol. Case Reports 6, 1–4.
Gill, C.M., Dolan, L., Piggott, L.M., McLaughlin, A.M., 2022. New developments in tuberculosis diagnosis and treatment. Breathe 18, 1–15.
Gler, M.T., Guilatco, R., Caoili, J.C., Ershova, J., Cegielski, P., Johnson, J.L., 2013. Weight Gain and response to treatment for multidrug-resistant tuberculosis. Am. J. Trop. Med. Hyg. 89, 943–949.
Goletti, D., Pisapia, R., Fusco, F.M., Aiello, A., Van Crevel, R., 2023. Epidemiology, pathogenesis, clinical presentation and management of TB in patients with HIV and diabetes. Int. J. Tuberc. Lung Dis. 27, 284–290.
Gopalaswamy, R., Dusthackeer, V.N.A., Kannayan, S., Subbian, S., 2021. Extrapulmonary Tuberculosis—An Update on the Diagnosis, Treatment and Drug Resistance. J. Respir. 1, 141–164.
Gupta, K.B., Gupta, R., Atreja, A., Verma, M., Vishvkarma, S., 2009. Tuberculosis and nutrition. Lung India 26, 9–16.
Gurung, L.M., Bhatt, L.D., Karmacharya, I., Yadav, D.K., 2018. Dietary Practice and Nutritional Status of Tuberculosis Patients in Pokhara: A Cross Sectional Study. Front. Nutr. 5, 3–8.
Heemskerk, D., Caws, M., Marais, B., Farrar, J., 2015. Tuberculosis in Children and Adults, First. ed, The Lancet. Springer International Publishing, New York, US.
Hickey, A.J., Gounder, L., Moosa, M.Y.S., Drain, P.K., 2015. A systematic review of hepatic tuberculosis with considerations in human immunodeficiency virus co-infection. BMC Infect. Dis. 15, 1–11.
Hoa, N.B., Lauritsen, J.M., Rieder, H.L., 2013. Changes in body weight and tuberculosis treatment outcome in Viet Nam. Int. J. Tuberc. Lung Dis. 17, 61–66.
Hung, N.T., Nga, N.T.H., Hung, L.X., Thao, N.P., Cuong, N.K., Nhung, L.T.T., 2023. Nutritional status and dietary intake before hospital admission of pulmonary tuberculosis patients. AIMS Public Heal. 10, 443–455.
Iradukunda, A., Ndayishimiye, G.P., Sinarinzi, D., Odjidja, E.N., Ntakaburimvo, N., Nshimirimana, I., Izere, C., 2021. Key factors influencing multidrug-resistant tuberculosis in patients under anti-tuberculosis treatment in two centres in Burundi: a mixed effect modelling study. BMC Public Health 21, 1–9.
Kadyrov, M., Thekkur, P., Geliukh, E., Sargsyan, A., Goncharova, O., Kulzhabaeva, A., Kadyrov, Asel, Khogali, M., Harries, A.D., Kadyrov, Abdullaat, 2023. Contact Tracing and Tuberculosis Preventive Therapy for Household Child Contacts of Pulmonary Tuberculosis Patients in the Kyrgyz Republic: How Well Are We Doing? Trop. Med. Infect. Dis. 8.
Kalva, J., Babu, S.P., Narasimhan, P.B., Raghupathy, K., Ezhumalai, K., Knudsen, S., Horsburgh, C.R., Hochberg, N., Salgame, P., Roy, G., Ellner, J., Sarkar, S., 2023. Predictors of weight loss during the intensive phase of tuberculosis treatment in patients with drug-susceptible pulmonary tuberculosis in South India. J. Public Heal. (United Kingdom) 45, 545–552.
Khawbung, J.L., Nath, D., Chakraborty, S., 2021. Drug resistant Tuberculosis: A review. Comp. Immunol. Microbiol. Infect. Dis. 74, 101574.
Kumar, R., 2008. Reproductive tract tuberculosis and male infertility. Indian J. Urol. 24, 392–395.
Lange, C., Chesov, D., Heyckendorf, J., Leung, C.C., Udwadia, Z., Dheda, K., 2018. Drug-resistant tuberculosis: An update on disease burden, diagnosis and treatment. Respirology 23, 656–673.
Lewinsohn, D.M., Leonard, M.K., Lobue, P.A., Cohn, D.L., Daley, C.L., Desmond, E., Keane, J., Lewinsohn, D.A., Loeffler, A.M., Mazurek, G.H., O’Brien, R.J., Pai, M., Richeldi, L., Salfinger, M., Shinnick, T.M., Sterling, T.R., Warshauer, D.M., Woods, G.L., 2017. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children. Clin. Infect. Dis. 64, e1–e33.
Liebenberg, D., Gordhan, B.G., Kana, B.D., 2022. Drug resistant tuberculosis: Implications for transmission, diagnosis, and disease management. Front. Cell. Infect. Microbiol. 12, 1–18.
Loh, S.Y., Zakaria, R., Mohamad, N., 2023. Knowledge, Attitude, and Stigma on Tuberculosis and the Associated Factors for Attitude Among Tuberculosis Contacts in Malaysia. Medeni. Med. J. 38, 45–53.
Makaminan, M.A., Vallery, M., Tumbol, L., Sumampouw, J.E., 2022. Description of Liver Function on the Effect of Treatment on Pulmonary Tuberculosis Patients at the Manado City Health Center. In: THE 5th International Conference On Health Polytechnics Of Surabaya (ICOHPS). Surabaya, pp. 1–11.
Malenfant, J.H., Brewer, T.F., 2021. Rifampicin Mono-Resistant Tuberculosis - A Review of an Uncommon but Growing Challenge for Global Tuberculosis Control. Open Forum Infect. Dis. 8, 1–6.
Malini, H., Huriani, E., Lenggogeni, D.P., Herlina, S., 2021. Health education on multidrug-resistant tuberculosis prevention among tuberculosis patients. Int. J. Public Heal. Sci. 10, 27–32.
Marliana Nurprilinda, Fajar Lamhot Gultom, Kurniyanto, Praisela Syania H Nelwan, 2023. Overview of pulmonary tuberculosis and extra pulmonary tuberculosis at the Siloam MRCCC Semanggi cancer hospital in 2018-2020. World J. Biol. Pharm. Heal. Sci. 13, 065–077.
Munro, S.A., Lewin, S.A., Smith, H.J., Engel, M.E., Fretheim, A., Volmink, J., 2007. Patient adherence to tuberculosis treatment: A systematic review of qualitative research. PLoS Med. 4, 1230–1245.
Nahid, P., Pai, M., Hopewell, P.C., 2006. Advances in the diagnosis and treatment of tuberculosis. Proc. Am. Thorac. Soc. 3, 103–110.
Nguyen, K.H., Alcantara, C.A., Glassman, I., May, N., Mundra, A., Mukundan, A., Urness, B., Yoon, S., Sakaki, R., Dayal, S., Chowdhury, T., Harshavardhan, S., Ramanathan, V., Venketaraman, V., 2023. Cutaneous Manifestations of Mycobacterium tuberculosis: A Literature Review. Pathogens 12.
Octaviana, D., Pramatama Mars Wijayanti, S., Nurlaela, S., 2019. Impact of Health Education on Knowledge and Awareness of Multidrug-Resistant Tuberculosis in Banyumas Regency, Indonesia. J. Fak. Kesehat. Masy. 13, 37–42.
Prasad, R., Nikhil Gupta, Banka, A., 2018. Multidrug‑resistant tuberculosis/rifampicin‑resistant tuberculosis: Principles of management. Lung India 35, 41–46.
Putranto, A.S., Bakti, P.S., Mazni, Y., Jeo, W.S., Lalisang, T., 2018. Clinical Presentation of Abdominal Tuberculosis. New Ropanasuri J. Surg. 3, 13–15.
Ren, Z., Zhao, F., Chen, H., Hu, D., Yu, W., Xu, X., Lin, D., Luo, F., Fan, Y., Wang, H., Cheng, J., Zhao, L., 2019. Nutritional intakes and associated factors among tuberculosis patients: A cross-sectional study in China. BMC Infect. Dis. 19, 1–8.
Rock, R.B., Olin, M., Baker, C.A., Molitor, T.W., Peterson, P.K., 2008. Central nervous system tuberculosis: Pathogenesis and clinical aspects. Clin. Microbiol. Rev. 21, 243–261.
Salazar-Austin, N., Mulder, C., Hoddinott, G., Ryckman, T., Hanrahan, C.F., Velen, K., Chimoyi, L., Charalambous, S., Chihota, V.N., 2022. Preventive Treatment for Household Contacts of Drug-Susceptible Tuberculosis Patients. Pathogens 11, 1–13.
Seung, K.J., Keshavjee, S., Rich, M.L., 2015. Multidrug-Resistant Tuberculosis and Extensively Drug-Resistant Tuberculosis. Cold Spring Harb Perspect Med 5, a017863.
Sharan kumar, V.G., Pajanivel, R., Boratne, A. V., Vimal Raj, R., 2022. Impact of dietary counselling on the nutritional status and quality of life among pulmonary tuberculosis patients - A randomized control trial. Indian J. Tuberc. 69, 201–206.
Silva, D.R., Gazzana, M.B., de Tarso Roth Dalcin, P., 2012. Severe tuberculosis requiring ICU admission. J. Bras. Pneumol. 38, 386–394.
Simbwa, B.N., Katamba, A., Katana, E.B., Laker, E.A.O., Nabatanzi, S., Sendaula, E., Opio, D., Ictho, J., Lochoro, P., Karamagi, C.A., Kalyango, J.N., Worodria, W., 2021. The burden of drug resistant tuberculosis in a predominantly nomadic population in Uganda: a mixed methods study. BMC Infect. Dis. 21, 1–11.
Smith, I., 2003. Mycobacterium tuberculosis pathogenesis and molecular determinants of virulence. Clin. Microbiol. Rev. 16, 463–496.
Soeroto, A.Y., Nurhayati, R.D., Purwiga, A., Lestari, B.W., Pratiwi, C., Santoso, P., Kulsum, I.D., Suryadinata, H., Ferdian, F., 2022. Factors associated with treatment outcome of MDR/RR-TB patients treated with shorter injectable based regimen in West Java Indonesia. PLoS One 17.
Soeroto, A.Y., Pratiwi, C., Santoso, P., Lestari, B.W., 2021. Factors affecting outcome of longer regimen multidrug-resistant tuberculosis treatment in West Java Indonesia: A retrospective cohort study. PLoS One 16, 1–13.
Souza, L.L.L., Santos, F.L. dos, Crispim, J. de A., Fiorati, R.C., Dias, S., Bruce, A.T.I., Alves, Y.M., Ramos, A.C.V., Berra, T.Z., da Costa, F.B.P., Alves, L.S., Monroe, A.A., Fronteira, I., Arcêncio, R.A., 2021. Causes of multidrug-resistant tuberculosis from the perspectives of health providers: challenges and strategies for adherence to treatment during the COVID-19 pandemic in Brazil. BMC Health Serv. Res. 21, 1–10.
UK health Security Agency, 2023. Contact tracing strategies for detecting tuberculosis in people exposed to tuberculosis in low incidence countries A rapid review.
Van Crevel, R., Karyadi, E., Netea, M.G., Verhoef, H., Nelwan, R.H.H., West, C.E., Van Der Meer, J.W.M., 2002. Decreased plasma leptin concentrations in tuberculosis patients are associated with wasting and inflammation. J. Clin. Endocrinol. Metab. 87, 758–763.
Vasantha, M., Gopi, P.G., Subramani, R., 2009. Weight gain in patients with tuberculosis treated under directly observed treatment short-course (DOTS). Indian J. Tuberc. 56, 5–9.
Vernon A, Fielding K, Savic R, Dodd L, Nahid P, 2019. The importance of adherence in tuberculosis treatment clinical trials and its relevance in explanatory and pragmatic trials. PLoS Med. 16, e1002884.
Warmelink, I., Ten Hacken, N.H., Van Der Werf, T.S., Van Altena, R., 2011. Weight loss during tuberculosis treatment is an important risk factor for drug-induced hepatotoxicity. Br. J. Nutr. 105, 400–408.
Windiyaningsih, C., Badaruddin, H., 2021. Factors influenced of drug-resistant tuberculosis and non-drug-resistant tuberculosis patients in Pulmonary Hospital Dr. M. Goenawan Partowidigdo, Bogor district. Tarumanagara Med. J. 3, 238–248.
Yani, D.I., Islam, H.S., Sari, C.W.M., 2018. Diet in The Intensive Phase of Pulmonary Tuberculosis Patients. J. Nurs. Care 1, 119–128.
Zaleskis, R., 2005. Postgraduate Course ERS Copenhagen 2005 - The side-effects of TB therapy. Beathr 2, 69–73.
Downloads
Published
License
Copyright (c) 2024 Efyluk Garianto, Barkha Agung Priyanto, Benedictus Sebastian Aldorino, Berlian Rutana Pratiwi, Bima Lazuardi, Bimo Saefulloh Fattah, Yohana Octavianda

This work is licensed under a Creative Commons Attribution 4.0 International License.