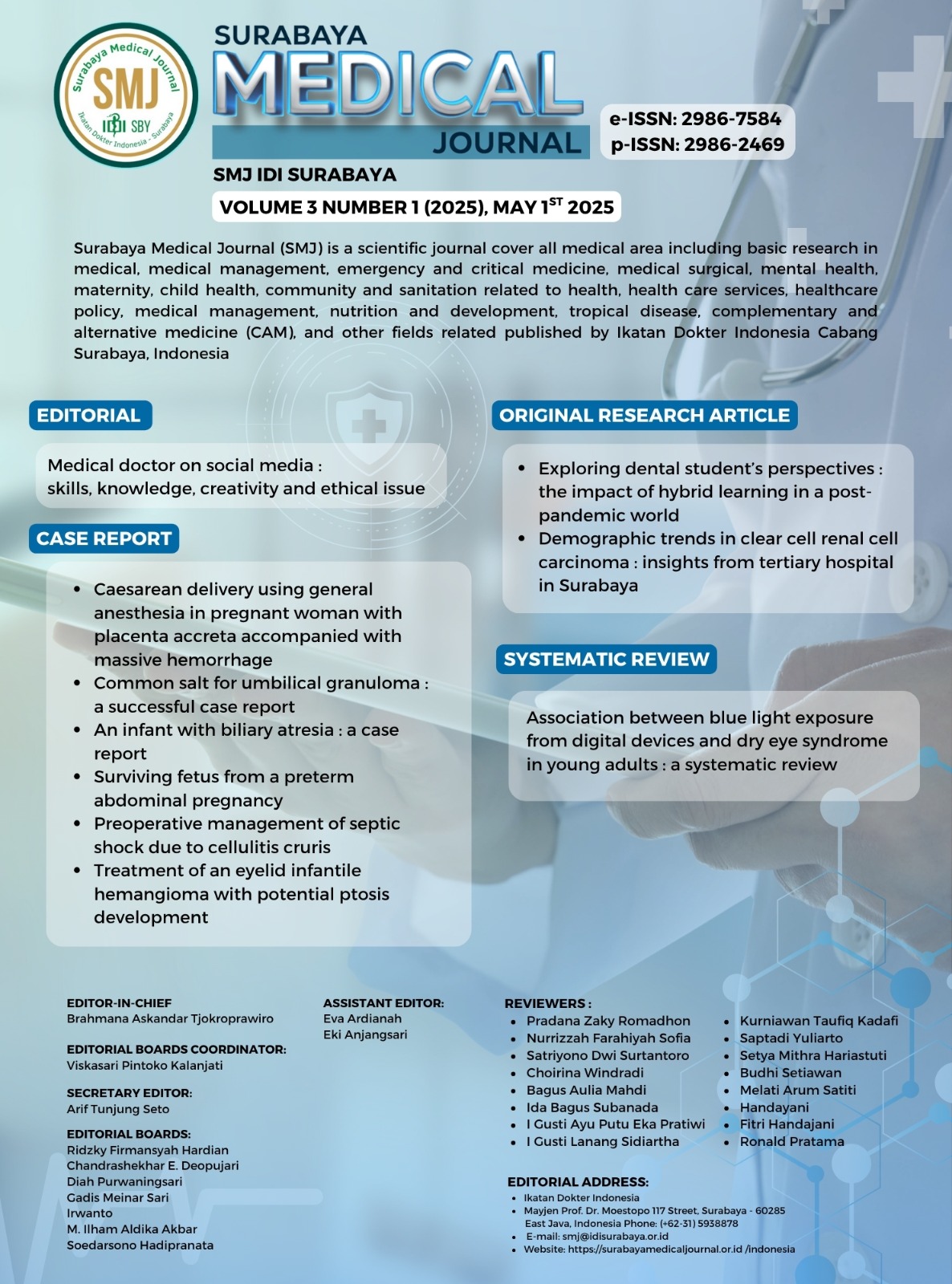
Preoperative management of septic shock due to cellulitis cruris
Management of septic shock in cellulitis cruris
DOI:
https://doi.org/10.59747/smjidisurabaya.v3i1.100Keywords:
Septic shock, cellulitis, acute kidney injury, debridement anesthesiaAbstract
Background: Septic shock is an emergency condition due to a systemic inflammatory response to infection, which can lead to multiple organ failure. Soft tissue infections such as cellulitis are one of the causes of sepsis, especially if not treated properly. Management of septic shock includes hemodynamic stabilization, antibiotic therapy, and control of the source of infection through debridement. The main challenge in this procedure is the risk of hemodynamic instability during anesthesia. Case Illustration: A 51-year-old man came with complaints of weakness and decreased consciousness, preceded by swelling and pain in the left leg. Examination showed septic shock with hypotension (69/45 mmHg), leukocytosis (34,000/µL), and AKI (creatinine 2.58 mg/dL). Fluid resuscitation and initial stabilization were performed before debridement. Anesthesia used total intravenous anesthesia (TIVA) with ketamine and sufentanil, and close monitoring with vasopressors. Conclusion: Management of septic shock due to cellulitis requires a multidisciplinary approach. Early stabilization, debridement, and appropriate anesthetic techniques play an important role in improving the patient's prognosis.
References
Ali, S., Athar, M., Ahmed, S.M., 2019. Basics of CPB. Indian J. Anaesth. 49, 257–262.
Bajracharya, G.R., Esa, W.A.S., Mao, G., Leung, S., Cohen, B., Maheshwari, K., Kessler, H.P., Gorgun, E., Sessler, D.I., Turan, A., 2023. Regional analgesia and surgical site infections after colorectal surgery: a retrospective cohort analysis. Brazilian J. Anesthesiol. (English Ed. 73, 10–15.
Bhagat, T.S., Kumar, L., Garg, P., Goel, A., Aggarwal, A., Gupta, S., 2023. To Study the Clinical Profile and Management of Cellulitis of Lower Limb in Northern India. Int. J. Low. Extrem. Wounds 22, 44–47.
Borguezam, C.B., Sanches, C.T., Albaneser, S.P.R., Moraes, U.R. de O., Grion, C.M.C., Kerbauy, G., 2021. Managed clinical protocol: impact of implementation on sepsis treatment quality indicators. Rev. Bras. Enferm. 74, 1–7.
Coopersmith, C.M., De Backer, D., Deutschman, C.S., Ferrer, R., Lat, I., Machado, F.R., Martin, G.S., Martin-Loeches, I., Nunnally, M.E., Antonelli, M., Evans, L.E., Hellman, J., Jog, S., Kesecioglu, J., Levy, M.M., Rhodes, A., 2018. Surviving sepsis campaign: research priorities for sepsis and septic shock. Intensive Care Med. 44, 1400–1426.
Dolin, H.H., Papadimos, T.J., Chen, X., Pan, Z.K., 2019. Characterization of Pathogenic Sepsis Etiologies and Patient Profiles: A Novel Approach to Triage and Treatment. Microbiol. Insights 12, 117863611882508.
Evans, L., Rhodes, A., Alhazzani, W., Antonelli, M., Coopersmith, C.M., French, C., Machado, F.R., Mcintyre, L., Ostermann, M., Prescott, H.C., Schorr, C., Simpson, S., Wiersinga, W.J., Alshamsi, F., Angus, D.C., Arabi, Y., Azevedo, L., Beale, R., Beilman, G., Belley-Cote, E., Burry, L., Cecconi, M., Centofanti, J., Yataco, A.C., Waele, J. De, Dellinger, R.P., 2021. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 49, e1063–e1143.
Font, M.D., Thyagarajan, B., Khanna, A.K., 2020. Sepsis and Septic Shock – Basics of diagnosis, pathophysiology and clinical decision making. Med. Clin. North Am. 104, 573–585.
Freise, H., Daudel, F., Grosserichter, C., Lauer, S., Hinkelmann, J., Van Aken, H.K., Sielenkaemper, A.W., Westphal, M., Fischer, L.G., 2009. Thoracic epidural anesthesia reverses sepsis-induced hepatic hyperperfusion and reduces leukocyte adhesion in septic rats. Crit. Care 13, 1–8.
Grondman, I., Pirvu, A., Riza, A., Ioana, M., Netea, M.G., 2020. Biomarkers of inflammation and the etiology of sepsis CHAPTER. Biochem Soc Trans 48, 1–23.
Guarino, M., Perna, B., Cesaro, A.E., Maritati, M., Spampinato, M.D., Contini, C., De Giorgio, R., 2023. 2023 Update on Sepsis and Septic Shock in Adult Patients: Management in the Emergency Department. J. Clin. Med. 12.
Gunderson, C.G., 2011. Cellulitis: Definition, etiology, and clinical features. Am. J. Med. 124, 1113–1122.
Gyawali, B., Ramakrishna, K., Dhamoon, A.S., 2019. Sepsis: The evolution in definition, pathophysiology, and management. SAGE Open Med. 7, 1–13.
Hakkarainen, T.W., Kopari, N.M., Pham, T.N., Evans, H.L., 2014. Necrotizing soft tissue infections: Review and current concepts in treatment, systems of care, and outcomes. Curr Probl Surg 51, 344–62.
Howell, M.D., Davis, A.M., 2017. Management of sepsis and septic shock. JAMA - J. Am. Med. Assoc. 317, 847–848.
Jarczak, D., Kluge, S., Nierhaus, A., 2021. Sepsis—Pathophysiology and Therapeutic Concepts. Front. Med. 8, 1–22.
Jia, Y., Burden, J., Lawton, T., Habli, I., 2020. Safe Reinforcement Learning for Sepsis Treatment. 2020 IEEE Int. Conf. Healthc. Informatics, ICHI 2020.
Kamath, S., Hammad Altaq, H., Abdo, T., 2023. Management of Sepsis and Septic Shock: What Have We Learned in the Last Two Decades? Microorganisms 11.
Kaur, N., 2022. Study of prognostic outcome of cellulitis patients with diabetes mellitus. Int. Surg. J. 9, 1700.
Legese, M.H., Asrat, D., Swedberg, G., Hasan, B., Mekasha, A., Getahun, T., Worku, M., Shimber, E.T., Getahun, S., Ayalew, T., Gizachew, B., Aseffa, A., Mihret, A., 2022. Sepsis: emerging pathogens and antimicrobial resistance in Ethiopian referral hospitals. Antimicrob. Resist. Infect. Control 11, 1–16.
Martínez, M.L., Plata-Menchaca, E.P., Ruiz-Rodríguez, J.C., Ferrer, R., 2020. An approach to antibiotic treatment in patients with sepsis. J. Thorac. Dis. 12, 1007–1021.
Myburgh, J.A., Chapman, M.J., Szekely, S.M., Osborne, G.A., 2005. Crisis management during anaesthesia: sepsis. Qual. Saf. Health Care 14, 1–4.
Park, C., Ku, N.S., Park, D.W., Park, J.H., Ha, T.S., Kim, D.W., Park, S.Y., Chang, Y., Jo, K.W., Baek, M.S., Seo, Y., Shin, T.G., Yu, G., Lee, J., Choi, Y.J., Jang, J.Y., Jung, Y.T., Jeong, I., Cho, H.J., Woo, A., Kim, S., Bae, D.H., Kang, S.W., Park, S.H., Suh, G.Y., Park, S., 2024. Early management of adult sepsis and septic shock: Korean clinical practice guidelines. Acute Crit. Care 39, 445–472.
Seymour, C.W., Liu, V.X., Iwashyna, T.J., Brunkhorst, F.M., Rea, T.D., Scherag, A., Rubenfeld, G., Kahn, J.M., Shankar-Hari, M., Singer, M., Deutschman, C.S., Escobar, G.J., Angus, D.C., 2016. Assessment of clinical criteria for sepsis for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA - J. Am. Med. Assoc. 315, 762–774.
Singer, M., Deutschman, C.S., Seymour, C., Shankar-Hari, M., Annane, D., Bauer, M., Bellomo, R., Bernard, G.R., Chiche, J.D., Coopersmith, C.M., Hotchkiss, R.S., Levy, M.M., Marshall, J.C., Martin, G.S., Opal, S.M., Rubenfeld, G.D., Poll, T. Der, Vincent, J.L., Angus, D.C., 2016. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA - J. Am. Med. Assoc. 315, 801–810.
Soumya, M., Singam, A., 2023. Comparative Study of Propofol with Ketamine and Propofol with Butorphanol for Total Intravenous Anesthesia in Short Surgical Procedures. Pravara Med. Rev. 45, 17–29.
Spiegel, R., Hockstein, M., 2022. The Survival of the Surviving Sepsis Campaign. Med Clin N Am 106, 1109–1117.
Sullivan, T., De Barra, E., 2018. Diagnosis and management of cellulitis. Clin. Med. J. R. Coll. Physicians London 18, 160–163.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Christopher Edwin Marijono, Yudianto Yudianto

This work is licensed under a Creative Commons Attribution 4.0 International License.