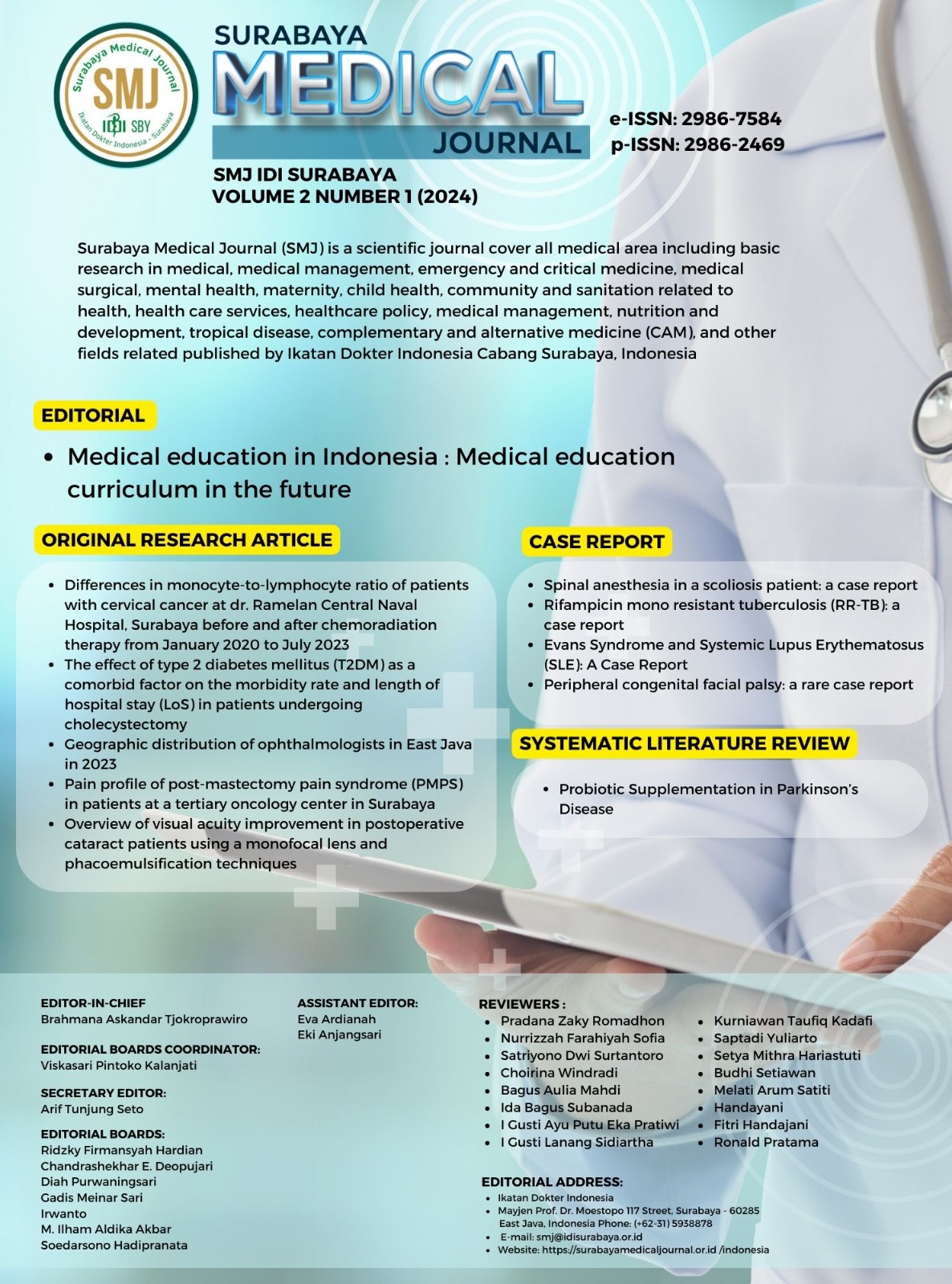
Geographic distribution of ophthalmologist in East Java 2023
Geographic distribution of ophthalmologist
DOI:
https://doi.org/10.59747/smjidisurabaya.v2i1.57Keywords:
ophthalmologist distribusion, epidemiology, public health, health system accessAbstract
Background: Based on the results of the Rapid Assessment of Avoidable Blindness conducted across 15 provinces in Indonesia, East Java has the greatest prevalence rate of blindness in Indonesia with 4.4% of the population affected and 81.1% of cases attributed to cataracts. Enhancing the human resource capacity is essential for managing visual impairment. It is necessary to ensure the strategic distribution of ophthalmologists in accordance with the needs and healthcare accessibility of the population. Objectives: This study aims to determine the geographic distribution of ophthalmologists in East Java and to investigate the correlation between the geographic distribution and various socio-economic indicators. Materials and Methods: This study was conducted from December 2023 to January 2024. The researchers used hospital websites and social media platforms to collect data on ophthalmologists at each hospital in East Java, with a ratio of one ophthalmologist per 20,000 population. The Pearson correlation test in SPSS version 27 was used to analyze the correlation between the ratio of ophthalmologists per 20,000 population and the human development index, health index, purchase power index, and education index of each region. Results: In this study, the estimated number of ophthalmologists in East Java in 2023 was 505, which ranged from one in Sampang Regency to 142 in Surabaya City. The regions with the highest ratio of ophthalmologists were Mojokerto, Surabaya, and Malang Cities. The ophthalmologists were concentrated in major urban centers, with a notable absence in rural areas. A significant correlation was identified between the ratio of ophthalmologists and the human development index, education index, purchase power index, health index, and regional minimum wage. Conclusion: The distribution of ophthalmologists in East Java remains imbalanced, with a concentration in major urban centers and a scarcity in rural areas. The ratio of ophthalmologists showed a significant correlation with socio-economic factors, including the human development index, education index, health index, purchase power index, and regional minimum wage.
References
Akosman, S., Tran, E., Rosenberg, S., Pakhchanian, H., Raiker, R., & Belyea, D. A. (2023). Patient Demand for Ophthalmologists in the United States: A Google Trends Analysis. Ophthalmic Epidemiology. https://doi.org/10.1080/09286586.2023.2273508
Allen, P., Jessup, B., Khanal, S., Baker-Smith, V., Obamiro, K., & Barnett, T. (2021). Distribution and location stability of the australian ophthalmology workforce: 2014–2019. International Journal of Environmental Research and Public Health, 18(23). https://doi.org/10.3390/ijerph182312574
Badan Pusat Statistik. (2017). Propinsi Jawa Timur dalam Angka.
Carvalho, R. D. S., Diniz, A. S., Lacerda, F. M., & Mello, P. A. D. A. (2012). Gross Domestic Product (GDP) per capita and geographical distribution of ophthalmologists in Brazil. Arquivos Brasileiros de Oftalmologia, 75(6), 407–411. https://doi.org/10.1590/S0004-27492012000600007
Das, T., Ackland, P., Correia, M., Hanutsaha, P., Mahipala, P., Nukella, P. B., … Win, T. (2018). Is the 2015 eye care service delivery profile in Southeast Asia closer to universal eye health need! International Ophthalmology, 38(2), 469–480. https://doi.org/10.1007/s10792-017-0481-y
Estopinal, C. B., Ausayakhun, S., Ausayakhun, S., Jirawison, C., Joy Bhosai, S., Margolis, T. P., & Keenan, J. D. (2013). Access to ophthalmologic care in Thailand: A regional analysis. Ophthalmic Epidemiology, 20(5), 267–273. https://doi.org/10.3109/09286586.2013.821498
Feng, P. W., Ahluwalia, A., Feng, H., & Adelman, R. A. (2020). National Trends in the United States Eye Care Workforce from 1995 to 2017. American Journal of Ophthalmology, 218, 128–135. https://doi.org/10.1016/j.ajo.2020.05.018
Hong, H., Mújica, O. J., Anaya, J., Lansingh, V. C., López, E., & Silva, J. C. (2016). The Challenge of Universal Eye Health in Latin America: Distributive inequality of ophthalmologists in 14 countries. BMJ Open, 6(11), 1–10. https://doi.org/10.1136/bmjopen-2016-012819
Kemenkes RI. (2018). Peta Jalan Penanggulangan gangguan penglihatan di Indonesia Tahun 2017-2030. In 2018. Retrieved from http://www.p2ptm.kemkes.go.id/dokumen-ptm/buku-peta-jalan-penanggulangan-gangguan-penglihatan-di-indonesia-tahun-2017-2030
Lee, C. S., Su, G. L., Baughman, D. M., Wu, Y., & Lee, A. Y. (2017). Disparities in delivery of ophthalmic care; An exploration of public Medicare data. PLoS ONE, 12(8), 1–12. https://doi.org/10.1371/journal.pone.0182598
Lita, M., Rini, M., & Syumarti. (2019). Mapping Jawa Barat.
Rif’Ati, L., Halim, A., Lestari, Y. D., Moeloek, N. F., & Limburg, H. (2021). Blindness and Visual Impairment Situation in Indonesia Based on Rapid Assessment of Avoidable Blindness Surveys in 15 Provinces. Ophthalmic Epidemiology, 28(5), 408–419. https://doi.org/10.1080/09286586.2020.1853178
Sengo, D. B., Salamo, Z. M. A., dos Santos, I. I. d’Alva B., Mate, L. M., Chivinde, S. M., Moragues, R., … López-Izquierdo, I. (2023). Assessment of the distribution of human and material resources for eye health in the public sector in Nampula, Mozambique. Human Resources for Health, 21(1), 1–11. https://doi.org/10.1186/s12960-023-00812-w
Stern, J., Yasmin, S., Qureshi, M. B., & Bourne, R. (2023). 2030 In Sight: the future of global eye health. Eye (Basingstoke), (September), 3–4. https://doi.org/10.1038/s41433-023-02815-2
Sun, Y., Chen, A., Zou, M., Zhang, Y., Jin, L., Li, Y., … Congdon, N. (2022). Time trends, associations and prevalence of blindness and vision loss due to glaucoma: An analysis of observational data from the Global Burden of Disease Study 2017. BMJ Open, 12(1), 1–6. https://doi.org/10.1136/bmjopen-2021-053805
United Nations Development Programme. (2020). Human Development Report: Technical Notes. In UNDP Organization. Retrieved from https://hdr.undp.org/sites/default/files/data/2020/hdr2020_technical_notes.pdf
Wang, K. M., Tseng, V. L., Liu, X., Pan, D., Yu, F., Baker, R., … Coleman, A. L. (2022). Association Between Geographic Distribution of Eye Care Clinicians and Visual Impairment in California. JAMA Ophthalmology, 140(6), 577–584. https://doi.org/10.1001/jamaophthalmol.2022.1001
Zhang, X., Beckles, G. L., Chou, C. F., Saaddine, J. B., Wilson, M. R., Lee, P. P., … Geiss, L. S. (2013). Socioeconomic disparity in use of eye care services among US adults with age-related eye diseases: National health interview survey, 2002 and 2008. JAMA Ophthalmology, 131(9), 1198–1206. https://doi.org/10.1001/jamaophthalmol.2013.4694
Zhong, J., Wang, W., Wang, H., Huang, J., Li, T., Chen, J., … Chen, W. (2021). Distribution and determinants of hospital efficiency and relative productivity in county-level hospitals in rural China: An observational study. BMJ Open, 11(7), 1–9. https://doi.org/10.1136/bmjopen-2020-042326
Downloads
Published
License
Copyright (c) 2024 Khansa Dhea Salsabila, Tamara Aulia Fakhrinnisa, Uyik Unari

This work is licensed under a Creative Commons Attribution 4.0 International License.