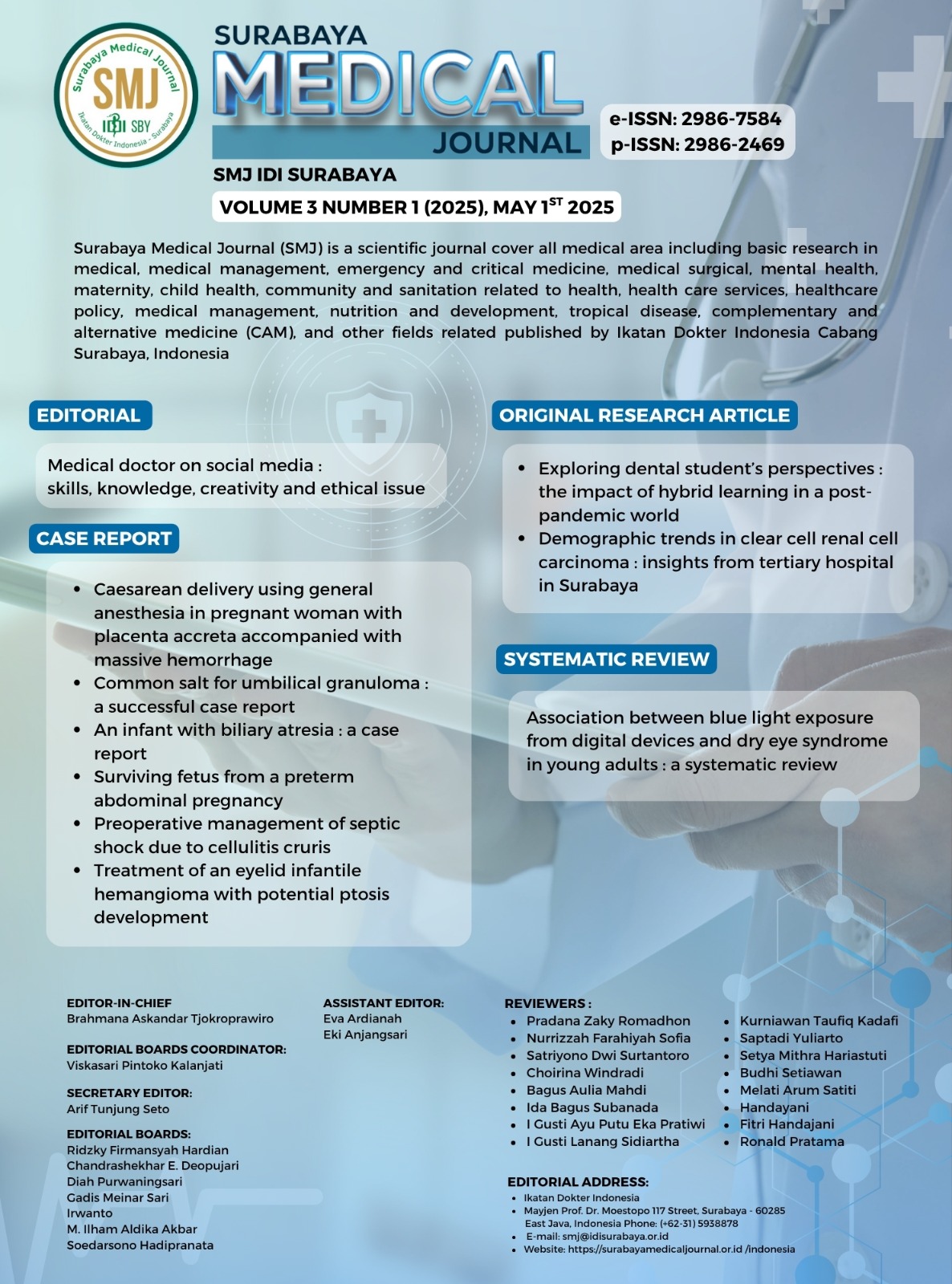
Caesarean delivery using general anesthesia in pregnant woman with placenta accreta accompanied with massive hemorrhage
Caesarean delivery in placenta accreta
DOI:
https://doi.org/10.59747/smjidisurabaya.v3i1.98Keywords:
General anesthesia, placenta accreta, caesarean delivery, hypovolemic shockAbstract
Background: Placenta accreta spectrum (PAS) is a disorder of placental implantation that causes peripartum bleeding and is the main cause of maternal death. PAS has a high risk of intraoperative bleeding therefore blood preparation and transfusion are essential. Objective: To describe the medical management of obstetric emergency of caesarean surgery with hypovolemic shock underwent general anaesthesia in patient with placenta accreta. Case: A woman, 36 years old, diagnosed with G4P3A0, gestational age 27-28 weeks with placenta accreta with blood pressure of 63/43, heart rate of 135, respiratory rate (RR) of 30, SpO2 97% O2 non rebreathing oxygen mask (NRBM) 10 lpm, experiencing vaginal bleeding since 6 days, was planned for caesarean delivery with emergency surgery due to hypovolemic shock as the result of massive hemorrhage, anemia, leukopenia, and hyponatremia. PAS diagnosis was determined after ultrasound imaging. Operation duration was 3.5 hours, with blood loss of 3,500 ml. After the surgery, she was transferred to the Intensive Care Unit (ICU). General anesthesia was chosen to maintain hemodynamic stability. The medical decision for this case was caesarean hysterectomy with the placenta left in situ after delivery of the foetus. Conclusion: Successful management of placenta accreta with massive bleeding is the result of appropriate perioperative management, good preparation and teamwork.
References
Abuhamad, A., 2013. Morbidly adherent placenta. Semin. Perinatol. 37, 359–364.
Ali, S., Athar, M., Ahmed, S.M., 2019. Basics of CPB. Indian J. Anaesth. 49, 257–262.
Alves, Á., Silva, L., Costa, F., Rezende, G., 2021. Management of placenta accreta spectrum. Rev Bras Ginecol Obs. 43, 713–723.
American Society of Anesthesiologists, 2006. Practice Guidelines for Perioperative Blood Transfusion. Pract. Guidel. Anesth. 105, 198–208.
Arakaza, A., Zou, L., Zhu, J., 2023. Placenta Accreta Spectrum Diagnosis Challenges and Controversies in Current Obstetrics: A Review. Int. J. Womens. Health 15, 635–654.
Bartels, H.C., Postle, J.D., Downey, P., Brennan, D.J., 2018. Placenta accreta spectrum: A review of pathology, molecular biology, and biomarkers. Dis. Markers 2018, 1507674.
Boujida, S., M’Hamdi, O., Flissate, F., Baidada, A., Kharbach, A., 2022. Placenta percreta as a cause of uterine rupture in the second trimester: Case report. Int. J. Surg. Case Rep. 94, 107069.
Chou, M.M., Ho, E.S.C., Lee, Y.H., 2000. Prenatal diagnosis of placenta previa accreta by transabdominal color Doppler ultrasound. Ultrasound Obstet. Gynecol. 15, 28–35.
Crochetière, C., 2003. Obstetric emergencies. Anesthesiol. Clin. North America 21, 111–125.
DeSimone, R.A., Leung, W.K., Schwartz, J., 2018. Transfusion Medicine in a Multidisciplinary Approach to Morbidly Adherent Placenta: Preparing for and Preventing the Worst. Transfus. Med. Rev. 32, 244–248.
Einerson, B.D., Gilner, J.B., Zuckerwise, L.C., 2023. Placenta accreta spectrum, Obstet Gynecol.
Eller, A.G., Bennett, M.A., Sharshiner, M., Masheter, C., Soisson, A.P., Dodson, M., Silver, R.M., 2011. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet. Gynecol. 117, 331–337.
Ersoy, A.O., Ozler, S., Oztas, E., Ersoy, E., Kirbas, A., Danisman, N., 2016. The association between placenta previa and leukocyte and platelet indices - A case control study. Ginekol. Pol. 87, 367–371.
Esakoff, T.F., Sparks, T.N., Kaimal, A.J., Kim, L.H., Feldstein, V.A., Goldstein, R.B., Cheng, Y.W., Caughey, A.B., 2011. Diagnosis and morbidity of placenta accreta. Ultrasound Obstet. Gynecol. 37, 324–327.
Fanniyah, F., Hartono, R., 2022. Hypervolemic Hemodilution as a Management During Predicted Massive Bleeding Sectio Caesarea in Placenta Accreta Patient. J. Anaesth. Pain 3, 13–16.
Fiszer, E., Weiniger, C.F., 2022. Placenta accreta. A review of current anesthetic considerations. Best Pract. Res. Clin. Anaesthesiol. 36, 157–164.
Fonseca, A., Ayres de Campos, D., 2021. Maternal morbidity and mortality due to placenta accreta spectrum disorders. Best Pract. Res. Clin. Obstet. Gynaecol. 72, 84–91.
Fox, C.J., Cornett, E.M., Ghali, G.E., 2019. Catastrophic perioperative complications and management: A comprehensive textbook, Catastrophic Perioperative Complications and Management: A Comprehensive Textbook. Springer, Switzerland.
Gandhi, K.A., Jain, K., 2018. Management of anaesthesia for elective, low‑risk (Category 4) caesarean section. Indian J. Anaesth. 62, 667‑674.
Goh, W., Zalud, I., 2016. Placenta accreta: A review of the etiology, diagnosis, and management. Donald Sch. J. Ultrasound Obstet. Gynecol. 10, 352–363.
Hakak, S., McCaul, C., Crowley, L., 2018. The adequacy of a 6-hour fasting period in term pregnancy—a gastric ultrasound study. Br. J. Anaesth. 120, e1.
Hecht, J.L., Baergen, R., Ernst, L.M., Katzman, P.J., Jacques, S.M., Jauniaux, E., Khong, T.Y., Metlay, L.A., Poder, L., Qureshi, F., Rabban, J.T., Roberts, D.J., Shainker, S., Heller, D.S., 2020. Classification and reporting guidelines for the pathology diagnosis of placenta accreta spectrum (PAS) disorders: recommendations from an expert panel. Mod. Pathol. 33, 2382–2396.
Huang, G., Zhou, R., Hu, Y., 2014. A new suture technique for cesarean delivery complicated by hemorrhage in cases of placenta previa accreta. Int. J. Gynecol. Obstet. 124, 262–263.
Imoto, S., Takeda, A., Koyama, K., Taguchi, S., Horibe, K., Nakamura, H., 2010. Late occurrence of severe hyponatremia followed by extrapontine osmotic demyelination syndrome after successful conservative management of postpartum hemorrhage due to placenta accreta by uterine artery embolization. J. Matern. Neonatal Med. 23, 742–746.
Jauniaux, E., Chantraine, Frederic, Silver, R.M., Langhoff-Roos, J., Duncombe, G., Klaritsch, P., Chantraine, Frédéric, Kingdom, J., Grønbeck, L., Rull, K., Nigatu, B., Tikkanen, M., Sentilhes, L., Asatiani, T., Leung, W.C., AIhaidari, T., Brennan, D., Kondoh, E., Yang, J.I., Seoud, M., Jegasothy, R., Espino y Sosa, S., Jacod, B., D’Antonio, F., Shah, N., Bomba-Opon, D., Ayres-de-Campos, D., Jeremic, K., Kok, T.L., Soma-Pillay, P., Tul Mandić, N., Lindqvist, P., Arnadottir, T.B., Hoesli, I., Jaisamrarn, U., Al Mulla, A., Robson, S., Cortez, R., 2018a. FIGO consensus guidelines on placenta accreta spectrum disorders: Epidemiology. Int. J. Gynecol. Obstet. 140, 265–273.
Jauniaux, E., Collins, S., Burton, G.J., 2018b. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am. J. Obstet. Gynecol. 218, 75–87.
Jauniaux, E., Collins, S., Burton, G.J., 2018c. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am. J. Obstet. Gynecol. 218, 75–87.
Jauniaux, E., Jurkovic, D., 2012. Placenta accreta: Pathogenesis of a 20th century iatrogenic uterine disease. Placenta 33, 244–251.
Jelting, Y., Klein, C., Harlander, T., Eberhart, L., Roewer, N., Kranke, P., 2017. Preventing nausea and vomiting in women undergoing regional anesthesia for cesarean section: Challenges and solutions. Local Reg. Anesth. 10, 83–90.
Kang, J., Kim, H.S., Lee, E.B., Uh, Y., Han, K.H., Park, E.Y., Lee, H.A., Kang, D.R., Chung, I.B., Choi, S.J., 2020. Prediction model for massive transfusion in placenta previa during cesarean section. Yonsei Med. J. 61, 154–160.
Khokhar, R.S., Baaj, J., Khan, M.U., Dammas, F.A., Rashid, N., 2016. Placenta accreta and anesthesia: A multidisciplinary approach. Saudi J. Anaesth. 10, 332–334.
Knöfler, M., Pollheimer, J., 2013. Human placental trophoblast invasion and differentiation: A particular focus on Wnt signaling. Front. Genet. 4, 1–14.
Koesmarsono, B., Aryananda, R.A., Ariani, G., Mardiyana, L., 2022. Lifesaving diagnosis of placenta accreta spectrum using MRI: Report of five cases. Radiol. Case Reports 17, 1803–1809.
Kumari, M., Patel, A.D., Mashruwala, V., 2024. Case series on placenta accreta spectrum disorder and its management. Int. J. Reprod. Contraception, Obstet. Gynecol. 13, 1825–1830.
Kyozuka, H., Yamaguchi, A., Suzuki, D., Fujimori, K., Hosoya, M., Yasumura, S., Yokoyama, T., Sato, A., Hashimoto, K., Kawamoto, T., Saito, H., Kishi, R., Yaegashi, N., Mori, C., Ito, S., Yamagata, Z., Inadera, H., Kamijima, M., Nakayama, T., Iso, H., Shima, M., Hirooka, Y., Suganuma, N., Kusuhara, K., Katoh, T., 2019. Risk factors for placenta accreta spectrum: Findings from the Japan environment and Children’s study. BMC Pregnancy Childbirth 19, 1–7.
Ladella, S., Ng, S., 2021. First trimester diagnosis of placenta accreta spectrum resulting in spontaneous uterine rupture: A case report. J. Case Reports Images Obstet. Gynecol. 7, 1–1.
Laranjo, M., Aniceto, L., Domingues, C., Gonçalves, L., Fonseca, J., 2024. Managing Placenta Accreta and Massive Hemorrhage: A Case Report on Anesthetic and Surgical Interventions. Cureus 16.
Liu, X., Wang, Y., Wu, Y., Zeng, J., Yuan, X., Tong, C., Qi, H., 2021. What we know about placenta accreta spectrum (PAS). Eur. J. Obstet. Gynecol. Reprod. Biol. 259, 81–89.
Loukopoulos, T., Zikopoulos, A., Plachoura, M., Galani, A., Zikopoulos, K., Kolibianakis, E., 2023. Emergency Obstetric Hysterectomy after Conservative Management of Placenta Accreta. Case Rep. Obstet. Gynecol. 2023, 2420333.
Lucas, N., Rex, S., Devroe, S., 2024. Treatment modalities for placenta accreta spectrum. Lancet 403, 437.
Mehdi, D.M., Chandraharan, E., 2021. Diagnosis and Management of Shock in Postpartum Haemorrhage. Glob. Libr. Women’s Med. 1–17.
Metzger, L., Teitelbaum, M., Weber, G., Kumaraswami, S., 2021. Complex Pathology and Management in the Obstetric Patient: A Narrative Review for the Anesthesiologist. Cureus 13.
Miller, D.A., Chollet, J.A., Goodwin, T.M., 1997. Clinical risk factors for placenta previa-placenta accreta. Am. J. Obstet. Gynecol. 177, 210–214.
Mirani, P., Lestari, P.M., Murti, K., Liberty, I.A., Andrina, H., Kesty, C., Stevanny, B., 2023. Placenta accreta spectrum disorder: An updated literature review. J. Kedokt. dan Kesehat. Indones. 14, 344–456.
Mittal, P., Suri, J., Pruthi, N., Pandey, D., Bharti, R., 2019. Comparison of placenta accreta spectrum disorders diagnosed in intrapartum and antepartum period— A three year experience in a tertiary referral unit of India. Eur. J. Obstet. Gynecol. Reprod. Biol. 236, 41–45.
Murayama, Y., Seki, H., Takeda, S., 2021. Intra-arterial Balloon Occlusion to Reduce Operative Bleeding for Placenta Previa Accreta Spectrum. Surg. J. 07, S11–S19.
Neef, V., Flinspach, A.N., Eichler, K., Woebbecke, T.R., Noone, S., Kloka, J.A., Jennewein, L., Louwen, F., Zacharowski, K., Raimann, F.J., 2024. Management and Outcome of Women with Placenta Accreta Spectrum and Treatment with Uterine Artery Embolization. J. Clin. Med. 13, 1–13.
Ozdemir, A., Karli, P., 2019. Can leukocytosis foresee hysterectomy for placenta previa? Ann. Med. Res. 26, 1842.
Prayitno, F.F., Islamy, N., Hussein, M.Zu., Sayuti, M., 2020. Syok Hipovolemik pada Plasenta Previa. Medula 10, 251–256.
Reale, S.C., Farber, M.K., 2022. Management of patients with suspected placenta accreta spectrum. BJA Educ. 22, 43–51.
Samir, G.M., 2023. Updates in the perioperative management of postpartum hemorrhage. Ain-Shams J. Anesthesiol. 15.
Schneck, H., Scheller, M., 2000. Acid aspiration prophylaxis and caesarean section. Curr. Opin. Anaesthesiol. 13, 261–265.
Sharashchandra, K.V., Shivaraj, S.P., 2020. Intra operative allowable blood loss: Estimation made easy. MedPulse Int. J. Anesthesiol. 14, 27–31.
Sherer, D.M., Thompson, M., Field, A., Granderson, F., Dalloul, M., 2023. Extensive fundal placenta accreta spectrum (PAS) in a nulliparous patient with an unscarred uterus and systemic lupus erythematosus (SLE) necessitating cesarean hysterectomy at delivery. Radiol. Case Reports 18, 4057–4061.
Sherif, A., El, A., El, A., Ismail, M., El, A., Elsayed, E.M., Hussein, A.M., 2024. Predictive Value of Complete Blood Countparameters in Placenta Accreta. Evid. Based Women’s Heal. J. 14, 1–10.
Silver, R.M., Fox, K.A., Barton, J.R., Abuhamad, A.Z., Simhan, H., Huls, C.K., Belfort, M.A., Wright, J.D., 2015. Center of excellence for placenta accreta. Am. J. Obstet. Gynecol. 212, 561–568.
Sivasankar, C., 2012. Perioperative management of undiagnosed placenta percreta: Case report and management strategies. Int. J. Womens. Health 4, 451–454.
Snegovskikh, D., Clebone, A., Norwitz, E., 2011. Anesthetic management of patients with placenta accreta and resuscitation strategies for associated massive hemorrhage. Curr. Opin. Anaesthesiol. 24, 274–281.
Spahn, D.R., Bouillon, B., Cerny, V., Duranteau, J., Filipescu, D., Hunt, B.J., 2019. Guia europea sangrado y coagulación. Crit. care 23, 1–74.
Supraptomo, Rt., Allan, A.H., 2021. Anesthesia Management in Patient with Placenta Percreta Performed Intra-aortic Ballooning Caesarean Section. Solo J. Anesth. Pain Crit. Care 1, 16.
Takeda, S., Takeda, J., Makino, S., 2020. Cesarean Section for Placenta Previa and Placenta Previa Accreta Spectrum. Surg. J. 06, S110–S121.
Tarantino, F., Calì, G., 2021. Placenta Accreta: Management by Peridural Anesthesia. Clin. Manag. Issues 15, 1–7.
The Society of Gynecologic Oncology endorses, 2018. Placenta Accreta Spectrum. Obstet. Gynecol. 132, e259.
Ulkumen, B.A., Pala, H.G., Baytur, Y., 2014. Acute abdomen and massive hemorrhage due to placenta percreta leading to spontaneous uterine rupture in the second trimester. Saudi Med. J. 35, 1131–1132.
Usta, I.M., Hobeika, E.M., Abu Musa, A.A., Gabriel, G.E., Nassar, A.H., 2005. Placenta previa-accreta: Risk factors and complications. Am. J. Obstet. Gynecol. 193, 1045–1049.
Warrick, C.M., Rollins, M.D., 2018. Peripartum anesthesia considerations for placenta accreta. Clin. Obstet. Gynecol. 61, 808–827.
Wijaya, T., 2021. Total placenta previa with high-risk morbidly adherent placenta and transverse lie fetal position. Bali J. Anesthesiol. 5, 201–203.
Zhang, J., Xu, H., Xin, Y., Zhang, C., Liu, Z., Han, X., Liu, Q., Li, Y., Huang, Z., 2020. Assessment of the massive hemorrhage in placenta accreta spectrum with magnetic resonance imaging. Exp. Ther. Med. 19, 2367–2376.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Kiki Rizqiyatul Lailiyah, I Gede Sutaniyasa, Virda Maharani

This work is licensed under a Creative Commons Attribution 4.0 International License.