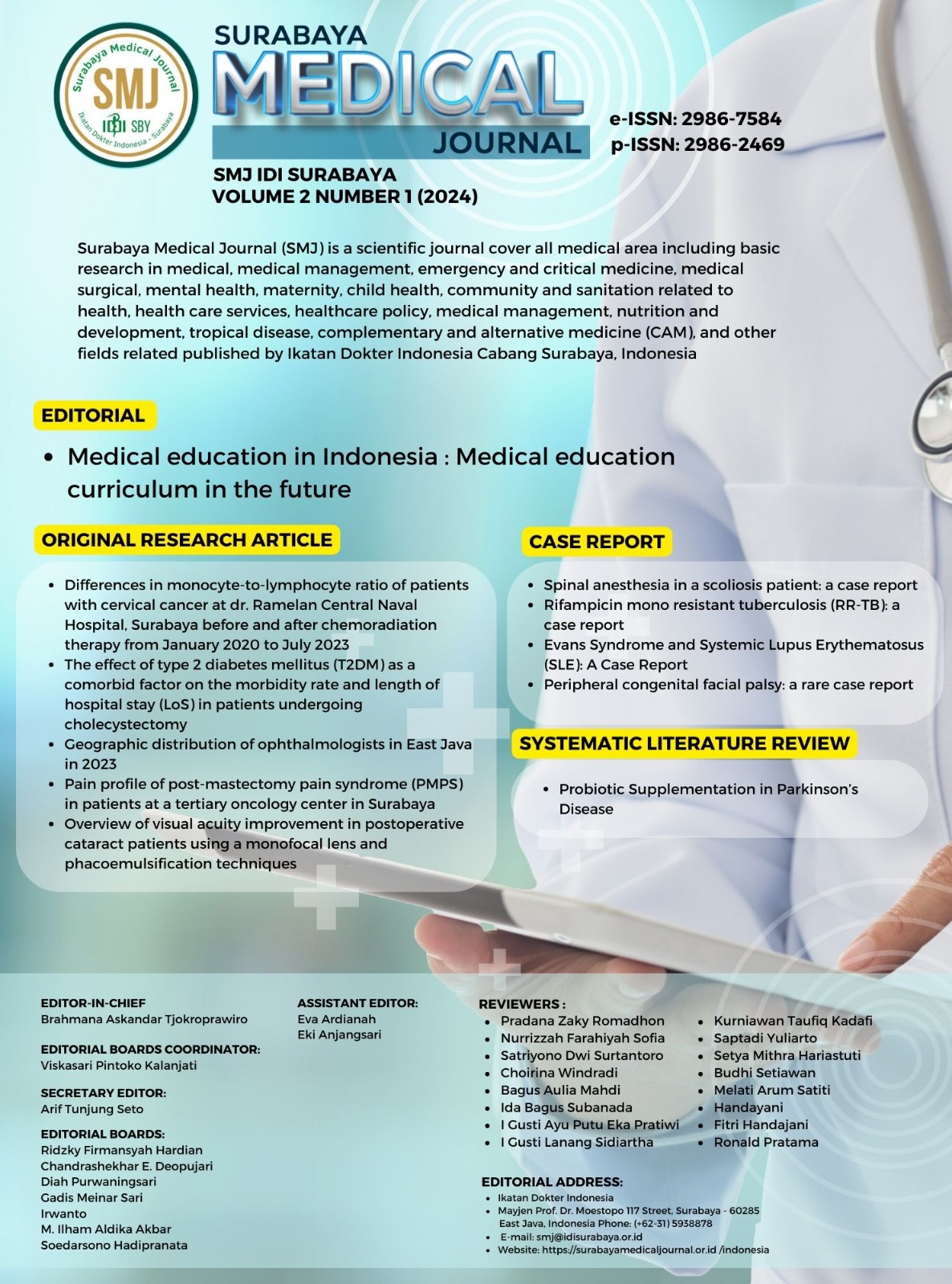
Peripheral congenital facial palsy: a rare case report
Congenital facial palsy in children
DOI:
https://doi.org/10.59747/smjidisurabaya.v2i1.52Kata Kunci:
congenital, facial palsy, neuropathy, rehabilitationAbstrak
Background: Congenital facial nerve palsy is a rare condition that is typically associated with a traumatic birth event or manifests as a characteristic of a syndrome that necessitates a rehabilitation program. Objective: This report aims to present a rare case and its subsequent outcome after undergoing a rehabilitation program. Case: An eight-month-old infant presented with complaints of an asymmetrical mouth when crying and smiling since birth. The left eye was unable to fully close. No evidence of a syndrome was found. The results of the electromyography of the left facial nerve revealed the presence of partial axonal loss, axonal malfunction, or neuropathy. The patient was subjected to a comprehensive treatment plan, involving rehabilitation programs such as neuromuscular electrical stimulation (NMES) and laser therapy over a period of 18 months. Discussion: It is important to determine if congenital facial palsy is a standalone condition or part of a broader syndrome. Rehabilitation programs, such as NMES and laser therapy, can stimulate the neurons and improve muscle weakness. The House-Brackmann scale demonstrated a clinical improvement, moving from grade V to grade II. With consistent physical therapy, the patient demonstrated improvements in facial expressions and eye closure. Conclusion: NMES and laser therapy, as well as facial massage and biofeedback, are potential treatments for congenital facial palsy due to their efficacy and favorable outcomes.
Referensi
Akter, D.J., Ara, P.D.B.H., Akter, P.D.D., Akter, D.M., Parvin, D.S., Afroje, D.S., 2022. Impact of COVID 19 on Preterm Rupture of Membrane. Sch. Int. J. Obstet. Gynecol. 5, 383–387.
Arya, S., Jain, S.K., Richardson, C.J., 2017. Facial Asymmetry in a Crying Newborn: A Comparison of Two Cases and Review of Literature. Case Rep. Pediatr. 2017, 1–3.
Baba, S., Kondo, K., Yoshitomi, A., Kanemaru, A., Nakaya, M., Yamasoba, T., 2021. Efficacy of Mirror Biofeedback Rehabilitation on Synkinesis in Acute Stage Facial Palsy in Children. Otol. Neurotol. 42, E936–E941.
Baelen, H., Esschendal, A.M., De Brucker, Y., Foulon, I., Topsakal, V., Gordts, F., 2023. Congenital facial nerve palsy: Single center study. In: Frontiers in Pediatrics. pp. 1–12.
Bharti, N., 2021. Role of Neuromuscular Electrical Stimulation in Bell’s Palsy: A Case Study of Three Patients. Int. J. Sci. Healthc. Res. 6, 235–241.
Bilge, S., Mert, G.G., Hergüner, M.Ö., İncecik, F., Sürmelioğlu, Ö., Bilen, S., Yılmaz, L., 2022. Peripheral facial nerve palsy in children: clinical manifestations, treatment and prognosis. Egypt. J. Neurol. Psychiatry Neurosurg. 58, 1–8.
Buhaibeh, Q., Madad, S., Dhaiban, T., 2019. Case report of Anotia with ipsilateral facial nerve palsy. Int. J. Res. Med. Sci. 7, 3583.
Ciorba, A., Corazzi, V., Conz, V., Bianchini, C., Aimoni, C., 2015. Facial nerve paralysis in children. World J. Clin. Cases 3, 973–979.
Clark, B.C., Mahato, N.K., Nakazawa, M., Law, T.D., Thomas, J.S., 2014. The power of the mind: The cortex as a critical determinant of muscle strength/weakness. J. Neurophysiol. 112, 3219–3226.
Coviello, C., Remaschi, G., Becciani, S., Montano, S., Corsini, I., Mussa, F., Basile, M., Dani, C., 2020. Erratum: Neonatal cerebellar hemorrhage and facial nerve palsy: An unusual association (AJP Reports (2020) 10:3 DOI: 10.1055/s-0040-1715162). AJP Rep. 10, E1.
Decraene, L., Boudewyns, A., Venstermans, C., Ceulemans, B., 2020. Developmental unilateral facial palsy in a newborn: six cases and literature review. Eur. J. Pediatr. 179, 367–375.
Dewi, N.M.R.P., Dharma, B.D.I., Silakarma, I.G.N.M.D., Samsarga, G.W., 2020. Multifaceted rehabilitation strategies for ramsay hunt syndrome: A case report and a review of literature. Bali Med. J. 9, 477–480.
Fargher, K.A., Coulson, S.E., 2017. Effectiveness of electrical stimulation for rehabilitation of facial nerve paralysis. Phys. Ther. Rev. 22, 169–176.
Ferreira, E.F., Portugal, D., Silva, N., Peixoto, C., Matos, C., Pereira, I., Prates, L., 2022. Rehabilitation of peripheral facial palsy associated with COVID-19 in a child: A case report. Ann. ofPhysical Rehabil. Med. 65, 101600.
Garro, A., Nigrovic, L.E., 2018. Managing Peripheral Facial Palsy. Ann. Emerg. Med. 71, 618–624.
Ho, M.L., Juliano, A., Eisenberg, R.L., Moonis, G., 2015. Anatomy and pathology of the facial nerve. Am. J. Roentgenol. 204, W612–W619.
Iacono, A., Pennisi, E., Benincasa, C., Marchetti, F., 2022. A case of facial nerve palsy in a pediatric patient associated with Covid-19. Ital. J. Pediatr. 48, 1–4.
Ivănescu, C.G., Dumitraș, S., Dimitriu, G., Turliuc, M., Crenguța, I., 2015. Journal of Clinical Research and Ophthalmology Goldenhar Syndrome. J. Clin. Res. Ophthalmol. 2, 041–044.
Kandakurti, P.K., Shanmugam, S., Basha, S.A., Amaravadi, S.K., Suganthirababu, P., Gopal, K., George, G.S., 2020. The effectiveness of low-level laser therapy combined with facial expression exercises in patients with moderate-to-severe Bell’s palsy: A study protocol for a randomised controlled trial. Int. J. Surg. Protoc. 24, 39–44.
Khair, A.M., Ibrahim, K., 2018. Idiopathic non-traumatic facial nerve palsy (Bell’s Palsy) in neonates; An atypical age and management dilemma. Oman Med. J. 33, 65–68.
Khurshid, A., Khurshid, M., Sohail, A., Raza, I.M., Ahsan, M.K., Alam Shah, M.U.F., Taseer, A.R., Nashwan, A.J., Ullah, I., 2022. Facial palsy as a manifestation of COVID-19: A systematic review of cases. Heal. Sci. Reports 5, 1–23.
Kim, J.H., Park, Y.C., Seo, B.K., Baek, Y.H., Goo, B., Nam, S.S., 2020. The efficacy of laser therapy in patients with facial palsy: A protocol for systematic review and meta-analysis. Med. (United States) 99, E21665.
Kumar, V., Narayanan, P., Shetty, S., Mohammed, A.P., 2021. Lower motor neuron facial palsy in a postnatal mother with COVID-19. BMJ Case Rep. 14, 10–12.
Mahale, R., Mehta, A., John, A., Buddaraju, K., Shankar, A., Rangasetty, S., 2016. Newborn with congenital facial palsy and bilateral anotia/atresia of external auditory canal: Rare occurrence. J. Pediatr. Neurosci. 11, 271–273.
Margono, R.S., Sukrisno, A., Nugrohowati, N., Lestari, W., 2021. Relationship Between A Premature Rupture Of Membranes And The Increase Of Leucocyte Levels In Pregnant Women During COVID-19 Pandemic. J. Kebidanan dan Kesehat. Tradis. 127–134.
Martinez-Perez, O., Prats Rodriguez, P., Muner Hernandez, M., Encinas Pardilla, M.B., Perez Perez, N., Vila Hernandez, M.R., Villalba Yarza, A., Nieto Velasco, O., Del Barrio Fernandez, P.G., Forcen Acebal, L., Orizales Lago, C.M., Martinez Varea, A., Muñoz Abellana, B., Suarez Arana, M., Fuentes Ricoy, L., Martinez Diago, C., Janeiro Freire, M.J., Alférez Alvarez-Mallo, M., Casanova Pedraz, C., Alomar Mateu, O., Lesmes Heredia, C., Wizner de Alva, J.C., Bernardo Vega, R., Macia Badia, M., Alvarez Colomo, C., Sanchez Muñoz, A., Pratcorona Alicart, L., Alonso Saiz, R., Lopez Rodriguez, M., del Carmen Barbancho Lopez, M., Meca Casbas, M.R., Vaquerizo Ruiz, O., Moran Antolin, E., Nuñez Valera, M.J., Fernandez Fernandez, C., Tubau Navarra, A., Cano Garcia, A.M., Baena Luque, C., Soldevilla Perez, S., Gastaca Abasolo, I., Adanez Garcia, J., Teulon Gonzalez, M., Puertas Prieto, A., Ostos Serna, R., del Pilar Guadix Martin, M., Catalina Coello, M., Ferriols Perez, E., Caño Aguilar, A., De la Cruz Conty, M.L., Sainz Bueno, J.A., 2021. The association between SARS-CoV-2 infection and preterm delivery: a prospective study with a multivariable analysis. BMC Pregnancy Childbirth 21, 1–11.
Mat Lazim, N., Ismail, H., Abdul Halim, S., Nik Othman, N.A., Haron, A., 2023. Comparison of 3 Grading Systems (House-Brackmann, Sunnybrook, Sydney) for the Assessment of Facial Nerve Paralysis and Prediction of Neural Recovery. Medeni. Med. J. 38, 111–119.
Meningaud, J.P., Pitak-Arnnop, P., Chikhani, L., Bertrand, J.C., 2006. Drooling of saliva: A review of the etiology and management options. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 101, 48–57.
Morea, A., Jessel, J., 2020. Comparing the effects of varied and constant preferred items on improving tummy time for typically developing infants. J. Appl. Behav. Anal. 53, 1367–1382.
Renault, F., Quijano-Roy, S., 2015. Congenital and Acquired Facial Palsies. In: Darras, B.T., Jones, H.R., Ryan, M.M., Vivo, D.C. De (Eds.), Neuromuscular Disorders of Infancy, Childhood, and Adolescence: A Clinician’s Approach. Academic Press, New York, US, pp. 225–242.
Saini, A., Singhi, P., Sodhi, K.S., Gupta, A., 2013. Bell palsy in a neonate with rapid response to oral corticosteroids: A case report. J. Child Neurol. 28, 506–508.
Shargorodsky, J., Lin, H.W., Gopen, Q., 2010. Facial nerve palsy in the pediatric population. Clin. Pediatr. (Phila). 49, 411–417.
Souni, G., Ayad, G., Elouali, A., Babakhouya, A., Rkain, M., 2023. Moebius Syndrome: A Case Report on an Uncommon Congenital Syndrome. Cureus 15, 1–4.
Sundari, S., Srinithi, R., 2022. A Case of Congenital Facial Nerve Palsy with Microtia. Int. J. Life Sci. Pharma Res. 12, 78–81.
Wen, J., 2022. Impact of COVID-19 pandemic on birth outcomes: A retrospective cohort study in Nanjing, China. Front. Public Heal. 10, 1–7.
Yuan, S.M., 2018. Nonsyndromic congenital absence of the pectoralis muscles. J. Nippon Med. Sch. 85, 246–249.
Zhang, W., Xu, L., Luo, T., Wu, F., Zhao, B., Li, X., 2020. The etiology of Bell’s palsy: a review. J. Neurol. 267, 1896–1905.
Unduhan
Diterbitkan
Lisensi
Hak Cipta (c) 2024 Masyithoh Budi Dewi, Donny Gunawan

Artikel ini berlisensi Creative Commons Attribution 4.0 International License.