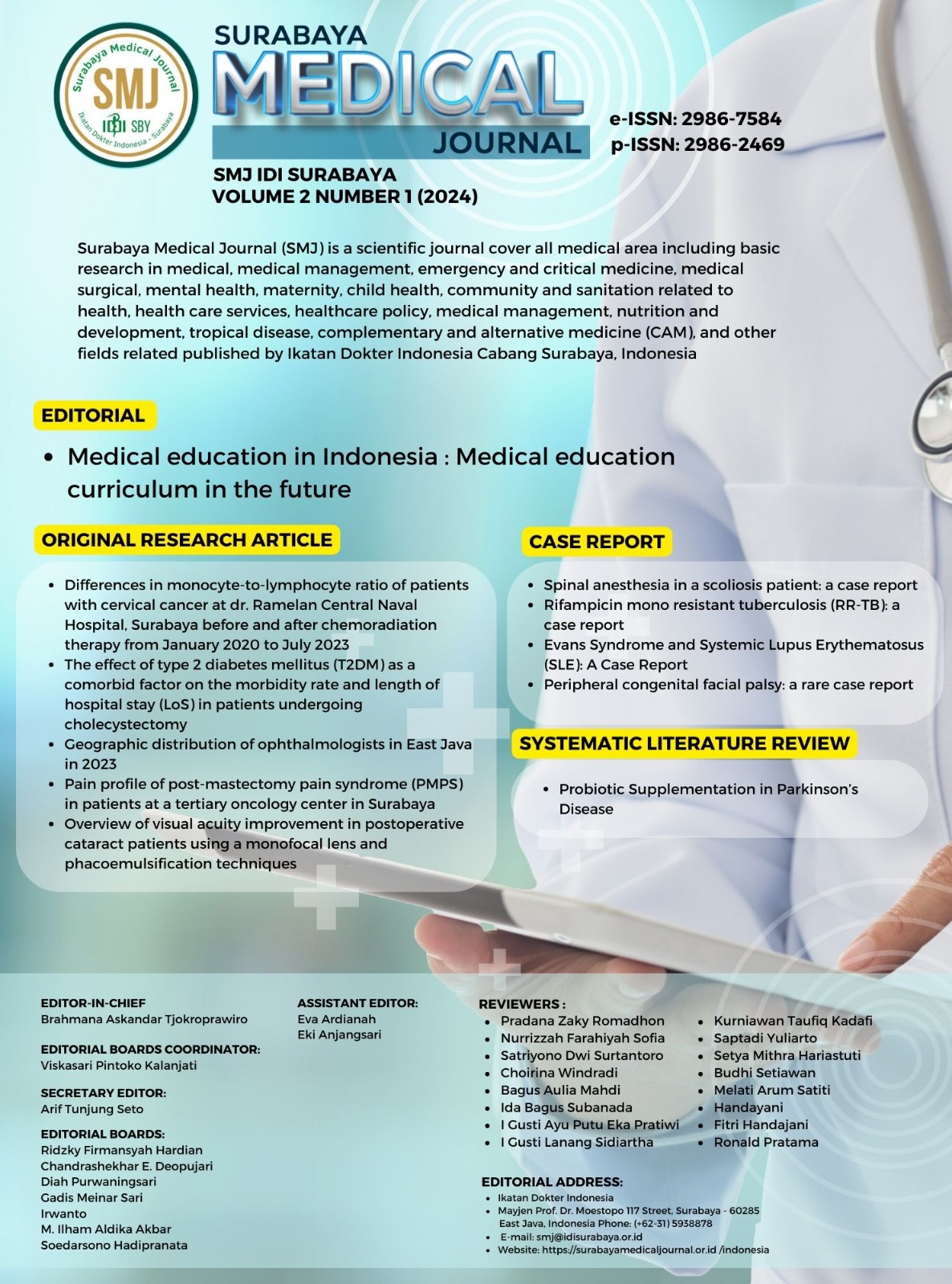
Evans syndrome and systemic lupus erythematosus (SLE): a case report
Evans syndrome and systemic lupus erythematosus
DOI:
https://doi.org/10.59747/smjidisurabaya.v2i1.66Kata Kunci:
Evans syndrome, immune thrombocytopenic purpura (ITP), autoimmune hemolytic anemia (AIHA), systemic lupus erythematosus (SLE)Abstrak
Background: Evans syndrome is a condition characterized by the simultaneous occurrence of immune thrombocytopenic purpura (ITP) and autoimmune hemolytic anemia (AIHA). The diagnosis of Evans syndrome presents a significant challenge due to its overlapping features with other autoimmune disorders. Objective: This case report aims to identify a diverse range of symptoms, including hematological and dermatological manifestations to provide a comprehensive diagnosis. In this case, the coexistence of fatigue, jaundice, pigmented macules, and papules led to the diagnosis of systemic lupus erythematosus (SLE) and Evans syndrome. Case: This case report presents a case of Evans syndrome in a 16-year-old female, delving into the intricate interplay of clinical manifestations and the potential association with SLE. The patient exhibited fatigue, pallor, jaundice, and dark-colored urine, along with the concurrent symptoms of dry cough and runny nose. A dermatological examination revealed hyperpigmented macules and papules on the face and extremities. Laboratory findings indicated severe anemia, thrombocytopenia, abnormal liver function, hyponatremia, and hypokalemia. The positive direct Coombs test and urinalysis findings supported the diagnoses of both Evans syndrome and SLE. The patient responded positively to systemic corticosteroid therapy and supportive care. Conclusion: This case underscores the diagnostic challenges associated with Evans syndrome, especially when overlapping with SLE. A multidisciplinary approach is crucial for accurate diagnosis and effective therapeutic interventions. Further research is necessary to unravel the complex relationships between these autoimmune diseases in cases of coexistence or overlap
Referensi
Aladjidi, N., Pincez, T., Rieux-Laucat, F., Nugent, D., 2023. Paediatric-onset Evans syndrome: Breaking away from refractory immune thrombocytopenia. Br. J. Haematol. 203, 28–35.
Audia, S., Grienay, N., Mounier, M., Michel, M., Bonnotte, B., 2020. Evans’ syndrome: From diagnosis to treatment. J. Clin. Med. 9, 1–22.
Cojocaru, M., Cojocaru, I.M., Silosi, I., Vrabie, C.D., 2011. Manifestations of Systemic Lupus Erythematosus. Medica 6, 330–336.
Couri, F.S., Kandula, M., 2020. A case of Evans syndrome with acute hemolysis and hemoglobin cast nephropathy. Am. J. Case Rep. 21, 1–4.
Fava, A., Petri, M., 2019. Systemic lupus erythematosus: Diagnosis and clinical management. J. Autoimmun. 96, 1–13.
Flores-Terry, M., García-Arpa, M., Anino-Fernández, J., MD, M.-S., 2017. Edematous Dermatomyositis with Probable Evans Syndrome. Actas Dermosifiliogr. 108, 673–675.
Giannouli, S., Voulgarelis, M., Ziakas, P.D., Tzioufas, A.G., 2006. Anaemia in systemic lupus erythematosus: from pathophysiology to clinical assessment. Ann Rheum Dis 65, 144–148.
Jaime-Pérez, J.C., Elva, P., Aguilar-Calderón, Salazar-Cavazos, L., Gómez-Almaguer, D., 2018. Evans syndrome: Clinical perspectives, biological insights and treatment modalities. J. Blood Med. 9, 171–184.
LaBere, B., Nguyen, A.A., Habiballah, S.B., Elkins, M., Imperial, J., Li, B., Devana, S., Timilsina, S., Stubbs, S.B., Joerger, J., Chou, J., Platt, C.D., 2023. Clinical utility of measuring CD4+ T follicular cells in patients with immune dysregulation. J. Autoimmun. 140.
Lao, C., White, D., Rabindranath, K., Van Dantzig, P., Foxall, D., Aporosa, A., Lawrenson, R., 2023. Incidence and prevalence of systemic lupus erythematosus in New Zealand from the national administrative datasets. Lupus 32, 1019–1027.
Liu, C.C., Ahearn, J.M., 2009. The search for lupus biomarkers. Best Pract. Res. Clin. Rheumatol. 23, 507–523.
Mendonca, S., Srivastava, S., Kapoor, R., Gupta, D., Gupta, P., Sharma, M.L., 2016. Evans syndrome and its link with systemic lupus erythematosus. Saudi J. Kidney Dis. Transpl. 27, 147–149.
Michel, M., Chanet, V., Dechartres, A., Morin, A.S., Piette, J.C., Cirasino, L., Emilia, G., Zaja, F., Ruggeri, M., Andrès, E., Bierling, P., Godeau, B., Rodeghiero, F., 2009. The spectrum of Evans syndrome in adults: New insight into the disease based on the analysis of 68 cases. Blood 114, 3167–3172.
Pope, J.E., 2002. Scleroderma overlap syndromes. Curr Opin Rheumatol. 14, 704–710.
Quintana-Ortega, C., Remesal, A., Vigara, A.P., Parrón-Pajares, M., Bret, M., Alcobendas, R., Murias, S., 2022. Severe thrombocytopenia as the main manifestation of childhood-onset systemic lupus erythematosus. Med. J. Nutrition Metab. 33, 223–226.
Skare, T., Picelli, L., dos Santos, T.A.G., Nisihara, R., 2017. Direct antiglobulin (Coombs) test in systemic lupus erythematosus patients. Clin. Rheumatol. 36, 2141–2144.
Stolyar, L., Rizi, B., Lin, S., Hsieh, E., 2019. Systemic lupus erythematosus presenting as Evans syndrome. Clin. Case Reports 7, 2513–2514.
Unduhan
Diterbitkan
Lisensi
Hak Cipta (c) 2024 Cheifia Krissanti Sasono, Myrna Saphira Fulca Fulca, Sarah Yunara Yunara

Artikel ini berlisensi Creative Commons Attribution 4.0 International License.